September and October have been very busy months for the team at TRBC! We are very proud to have won the Innovate Awards from The ASHN Network and NHS Confed. To help share information across a wider network of AHSN’s, we were asked to be involved in a Case Study, highlighting the community benefits of our innovation.
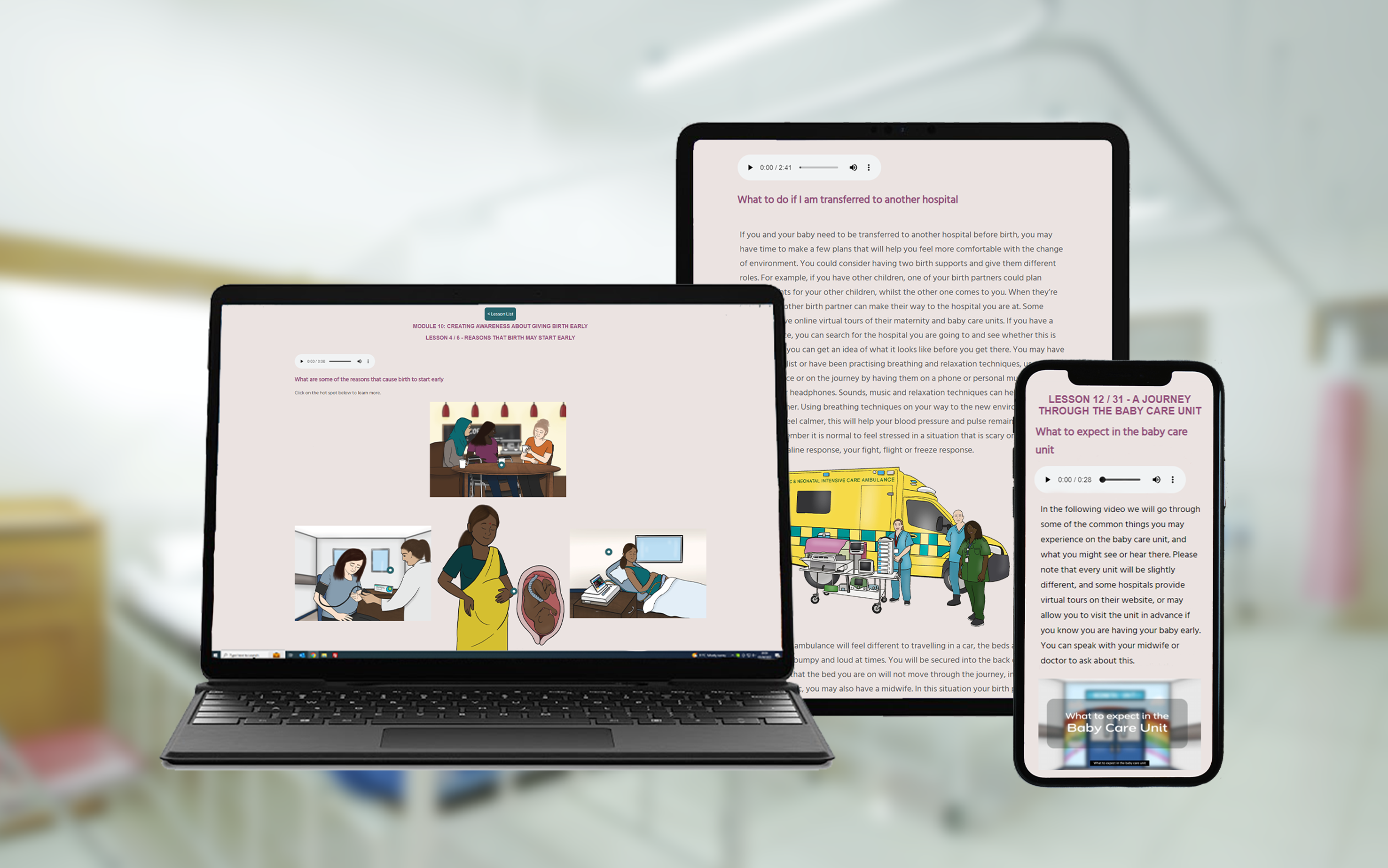
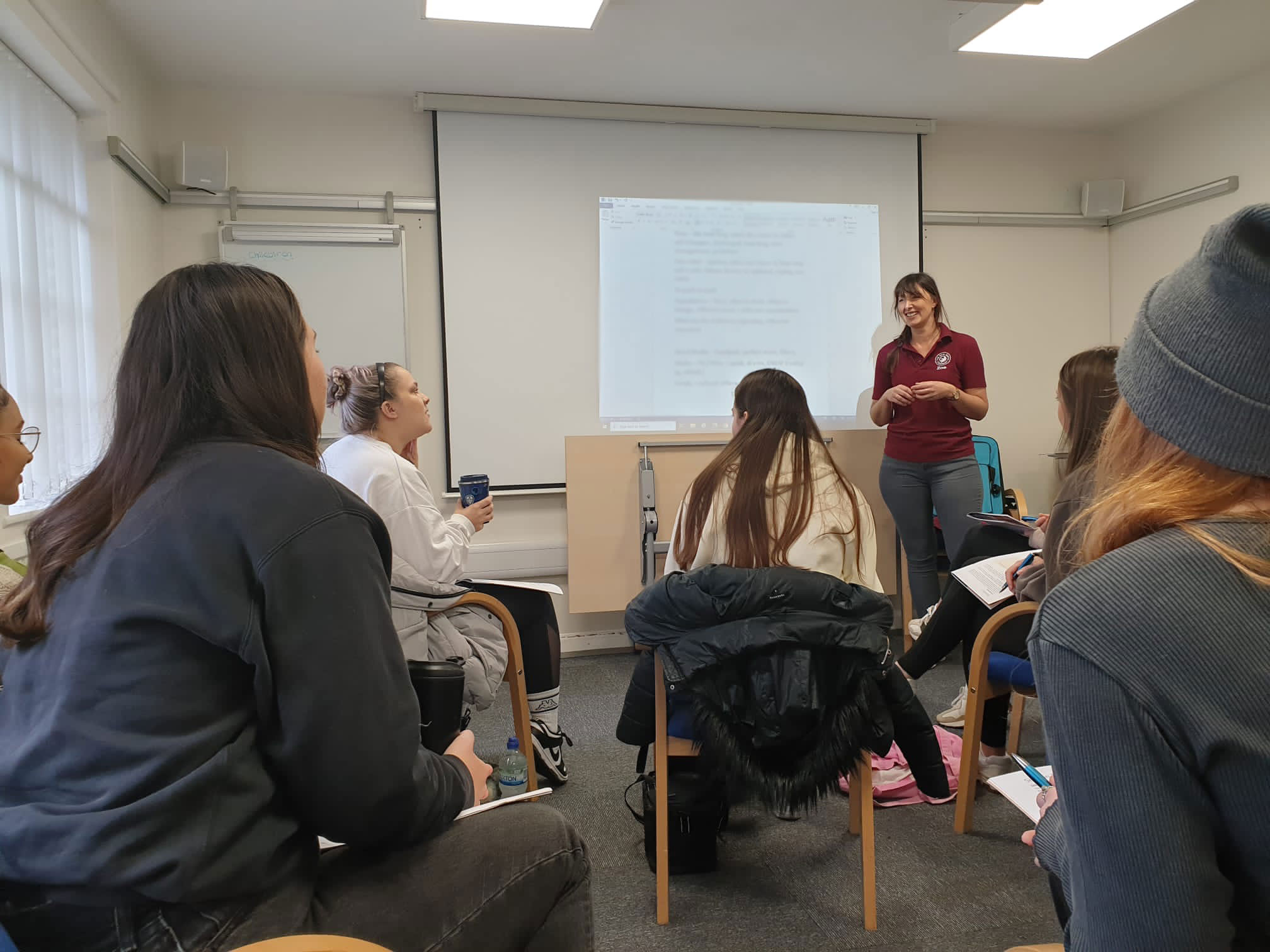
TRBC uses a combined approach of digital technology and midwifery training in our Real Birth Programme to enable equitable access to important birth preparation information that supports a deeper understanding of birth options. To support a better understanding of childbirth physiology, we provide a variety of visual and audio guides, whilst applying Human Factors in the creation and design.
Outcomes for maternity service users are increased awareness of options and choices – leading to better personalised conversations with their healthcare providers, reduced interventions in labour and better birth experiences for more women nationally.
The guideline provides five recommendations on interventions that should be applied outside of routine clinical interactions between a health care provider and pregnant woman. These include:
- Educational interventions for women and families to support meaningful dialogue with providers and informed decision-making on mode of delivery.
- Use of clinical guidelines, audits of caesarean sections, and timely feedback to health professionals about caesarean section practices.
- Requirement for second opinion for caesarean section indication at point of care in settings with adequate resources.
- Collaborative midwifery-obstetrician model of care or financial strategies, only under rigorous research.
- No intervention for labour induction or augmentation, labour ward management, or pain relief.
TRBC’s data from 2022 shows reductions in the rate of emergency caesarean birth and increased positive birth experiences in users of our Programme. Increasing equity has always been ‘the top priority’, as trends of increasing interventions can be seen in areas across the UK where access to information is limited due to lack of equitable resources. Resources that have been digitally translated have been found to be misleading and inaccurate , widening the equity gap.
We provide education and information to women and families about the benefits and risks of different options in childbirth and provide supportive tools that can help them make informed decisions.
We follow up by using data and indicators to monitor and evaluate the impact of the Programme on equity and equality, and share good practices and learning across the UK within adopted sites.
To read more about our approach you can read our case study here:
Essential digital support for mothers-to-be – The AHSN Network